Acute pancreatitis is a sudden inflammation of the pancreas that demands immediate attention, presenting a significant impact on an individual’s health and well-being. Understanding its complexity, from the initial signs of acute pancreatitis to the severe stages and potential life expectancy after recovery, underscores the importance of recognizing and addressing this condition promptly. We are poised to delve into the intricacies of acute pancreatitis, unraveling its pathophysiology, identifying the causes and risk factors, and exploring the symptoms that warrant medical intervention. Recognizing the urgency and severity that acute pancreatitis imposes is crucial in appreciating the depth of information we’ll explore, aiming to offer comprehensive insights into managing this life-threatening condition effectively.
In this article, we will guide you through the diagnosis of acute pancreatitis, emphasizing the crucial steps in identifying the condition accurately. Further, we’ll navigate the landscape of acute pancreatitis treatment, detailing the management strategies that can mitigate the complications associated with this ailment. From discussing the 4 stages of acute pancreatitis to addressing the challenges posed by necrotizing acute pancreatitis and chronic acute pancreatitis, our coverage will span the spectrum of the condition. Equally, by detailing the acute pancreatitis complications, we intend to arm readers with the knowledge needed to confront this ailment head-on, fostering a better understanding of the potential outcomes and the importance of effective treatment strategies in improving life expectancy after acute pancreatitis.
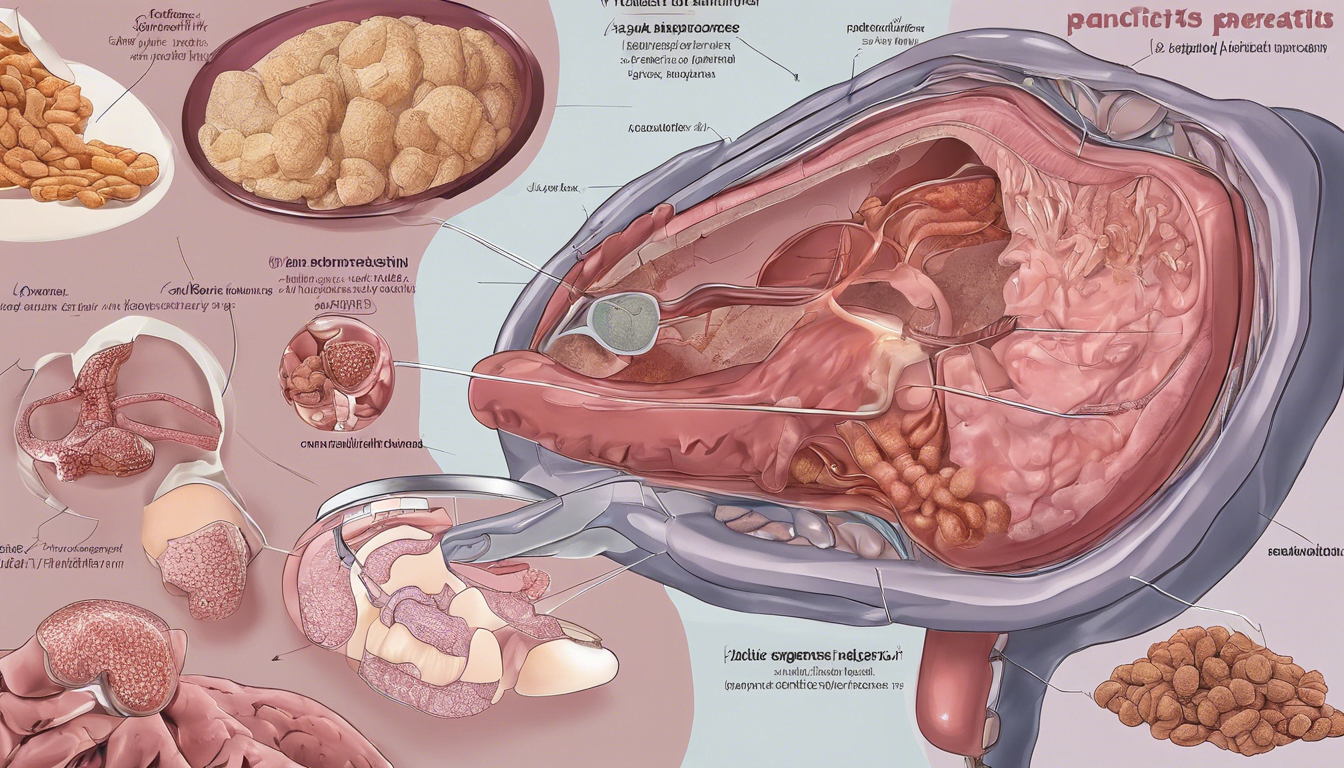
What is Acute Pancreatitis?
Acute pancreatitis is a condition characterized by the sudden inflammation of the pancreas, which can vary widely in severity from mild discomfort requiring minimal intervention to severe, life-threatening complications. This inflammation typically presents as a sharp, severe pain in the upper abdomen that may radiate to the back, often accompanied by nausea, vomiting, fever, and a rapid pulse.
The pancreas, located behind the stomach and in front of the spine, plays a crucial dual role in our digestive and endocrine systems. It produces enzymes that aid in the digestion of food and hormones like insulin that regulate blood sugar levels. Acute pancreatitis occurs when these digestive enzymes become activated while still in the pancreas, causing irritation and swelling of the pancreatic tissue.
We observe that acute pancreatitis is the most common cause of gastrointestinal-related hospital admissions in the United States, reflecting its significant impact on health. The causes of acute pancreatitis include gallstones, excessive alcohol consumption, and high levels of triglycerides in the blood, with the prevalence of each cause varying by geographic and socioeconomic factors.
The Atlanta classification system identifies two main types of acute pancreatitis: interstitial edematous pancreatitis, which involves inflammation and edema of the pancreatic tissue, and necrotizing pancreatitis, where there is tissue death within the pancreas. Depending on the severity, acute pancreatitis is classified into mild, moderately severe, and severe categories, which helps guide the treatment approach and management strategies.
In summary, acute pancreatitis represents a sudden inflammatory attack of the pancreas with a spectrum of clinical presentations and severities, necessitating prompt medical evaluation and care to prevent complications and ensure recovery.
Symptoms of Acute Pancreatitis
In our exploration of acute pancreatitis, we find that the symptoms of this condition can be quite severe and varied. The primary symptom most individuals experience is a significant pain in the upper belly, which often radiates to the back. This pain may intensify when touching the belly, indicating tenderness and inflammation of the pancreas.
Additionally, we often observe a rapid pulse and fever as common symptoms, reflecting the body’s response to inflammation. Nausea and vomiting are also frequent, which can complicate the clinical picture by causing dehydration and electrolyte imbalances.
In more severe cases, symptoms can include fast, shallow breathing, which may be a sign of the body trying to compensate for metabolic disturbances caused by the pancreas’ impaired function. Swelling and tenderness in the belly area are also indicative of the inflammation spreading and possibly affecting nearby organs.
Understanding these symptoms is crucial for timely diagnosis and management, as the severity and progression of symptoms can vary widely among individuals. We emphasize the importance of recognizing these signs early to initiate appropriate medical interventions and prevent complications.
Causes and Risk Factors of Acute Pancreatitis
Alcohol-related Causes
We find that chronic alcohol consumption is responsible for 17% to 25% of acute pancreatitis cases worldwide, making it the second most common cause after gallstones. The risk increases with the duration and amount of alcohol intake, particularly in individuals consuming approximately 4-5 drinks daily over five years or more. Notably, excessive alcohol use not only triggers acute episodes but also contributes to the progression towards chronic pancreatitis. Additionally, a recent study highlighted a significant 50% increase in deaths from alcohol-induced acute pancreatitis between 2019 and 2020, underscoring the severe impact of alcohol on pancreatic health.
Gallstone-related Causes
Gallstones are the primary cause of acute pancreatitis, implicated in 30% to 50% of cases. These stones, forming from crystalized bile components, can obstruct the bile duct, leading to a backup of pancreatic enzymes that inflame the pancreas. The blockage typically occurs when a gallstone gets lodged in the common bile duct, causing a significant increase in pressure that activates these enzymes prematurely. Surgical interventions, such as endoscopic retrograde cholangiopancreatography (ERCP), are often necessary to remove these obstructions and alleviate the condition.
Other Causes
Apart from alcohol and gallstones, acute pancreatitis can also arise from a variety of other factors. These include hypertriglyceridemia, drug-induced reactions, and post-procedural complications such as those following abdominal surgery or ERCP. Less common causes encompass genetic disorders, infections (viral or bacterial), and systemic conditions like autoimmune disorders or renal disease. Additionally, lifestyle factors like smoking significantly elevate the risk, with smokers being three times more likely to develop chronic pancreatitis compared to nonsmokers.
Diagnosis of Acute Pancreatitis
Clinical Examination
When diagnosing acute pancreatitis, our initial approach involves a thorough clinical examination. During this examination, we check for abdominal pain, swelling, or tenderness, which are common indicators of the condition. The presence of fever and a rapid pulse during the physical exam can also suggest an inflammatory process.
Laboratory Tests
We proceed with laboratory tests that are critical in confirming the diagnosis of acute pancreatitis. Key tests include measuring serum amylase and lipase levels, which are digestive enzymes produced by the pancreas. Levels that are three times higher than the normal range are indicative of acute pancreatitis. Additionally, we assess blood glucose, blood fats, and look for signs of infection or inflammation. These tests help us to not only confirm the diagnosis but also to understand the severity of the pancreatitis.
Imaging Tests
Imaging tests play a pivotal role in diagnosing acute pancreatitis and assessing its complications. We commonly use ultrasound and computed tomography (CT) scans as the primary imaging modalities. Ultrasound can help identify gallstones, a common cause of acute pancreatitis, while CT scans provide detailed images of the pancreas and surrounding structures, helping to confirm pancreatitis or detect pancreatic cancer. For more detailed visualization, especially to assess the bile ducts and pancreatic ducts, magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS) are employed. These advanced imaging techniques are crucial for a comprehensive assessment and to guide further management strategies.
Treatment and Management of Acute Pancreatitis
Initial Management
In cases of acute pancreatitis, initial management is crucial and typically begins with hospitalization to control symptoms and prevent complications. Our approach includes administering intravenous (IV) fluids to maintain hydration and using pain medications to manage severe abdominal pain. Nutrition is carefully managed, starting with nil per os (nothing by mouth) to reduce pancreatic stimulation, and gradually reintroducing oral feeding as tolerated. In more severe cases, enteral nutrition via a feeding tube may be necessary.
Ongoing Treatment
As the patient stabilizes, ongoing treatment focuses on addressing the underlying causes and managing complications. For gallstone-related pancreatitis, procedures like Endoscopic Retrograde Cholangiopancreatography (ERCP) are used to remove blockages from the bile or pancreatic ducts. In cases where alcohol consumption is the cause, programs for alcohol dependency treatment are recommended to prevent recurrence. Adjustments in medication may be required if drug-induced pancreatitis is suspected.
Surgical Interventions
Surgical interventions are considered when conservative treatments fail or complications arise. For patients with necrotizing pancreatitis, less invasive surgeries such as laparoscopic or endoscopic techniques are preferred to minimize recovery times and reduce complications. These may include transgastric or retroperitoneal approaches to remove necrotic tissue or drain fluid collections. Cholecystectomy, the surgical removal of the gallbladder, is often performed during the same hospital admission to prevent future episodes in cases of gallstone pancreatitis.
In managing acute pancreatitis, the timing of surgery is critical. Early surgery is avoided to allow for better delineation of necrotic tissues and to reduce the risk of complications.
Conclusion
Throughout the discourse on acute pancreatitis, we have traversed the breadth of its pathophysiology, delving into its diagnoses, causes, risk factors, and available treatments. The meticulous examination of the condition underscores the paramount importance of early recognition and intervention, which significantly influence the prognosis and quality of life of those affected. By charting the complex terrain of acute pancreatitis, from its symptoms to the multifaceted treatment approaches, this article aims to elevate awareness and understanding, providing a dependable resource for managing this acute condition effectively.
Understanding acute pancreatitis is crucial, not only for healthcare professionals but also for individuals who may be at risk. Our discussion reiterates the necessity for a comprehensive approach in addressing the causative factors, tailored management strategies, and the imperative for ongoing research and education in this domain. As we conclude, let this serve as a call to action for heightened vigilance and proactive management, ensuring better outcomes for those suffering from acute pancreatitis. The journey through understanding and managing acute pancreatitis is a testament to the resilience in confronting and overcoming the challenges posed by this life-threatening condition.