In facing the diagnosis of acute lymphocytic leukemia, patients and their loved ones often find themselves navigating a maze of medical information, seeking clarity on what lies ahead. This type of cancer, which rapidly affects the white blood cells, holds a myriad of complexities that can influence both treatment paths and outcomes. Our understanding of acute lymphocytic leukemia, including its subtypes such as B cell acute lymphocytic leukemia, has grown significantly, enabling more personalized and effective treatment options. It’s crucial for patients to arm themselves with essential knowledge about their condition, including the signs and symptoms, treatment strategies, and insights into the survival rate and prognosis, to make informed decisions about their care.
In this article, we aim to provide a comprehensive overview of acute lymphocytic leukemia, from its causes and risk factors to the latest in treatment options. We will explore the typical signs and symptoms that may indicate the presence of the disease, how it is diagnosed, and what patients can expect from the treatment process. Our discussion will further delve into the acute lymphocytic leukemia survival rate and prognosis, offering hope and guidance for those affected. By understanding these key aspects, patients and their families can better prepare for the journey ahead, equipped with the knowledge needed to navigate the challenges of acute lymphocytic leukemia.
What is Acute Lymphocytic Leukemia?
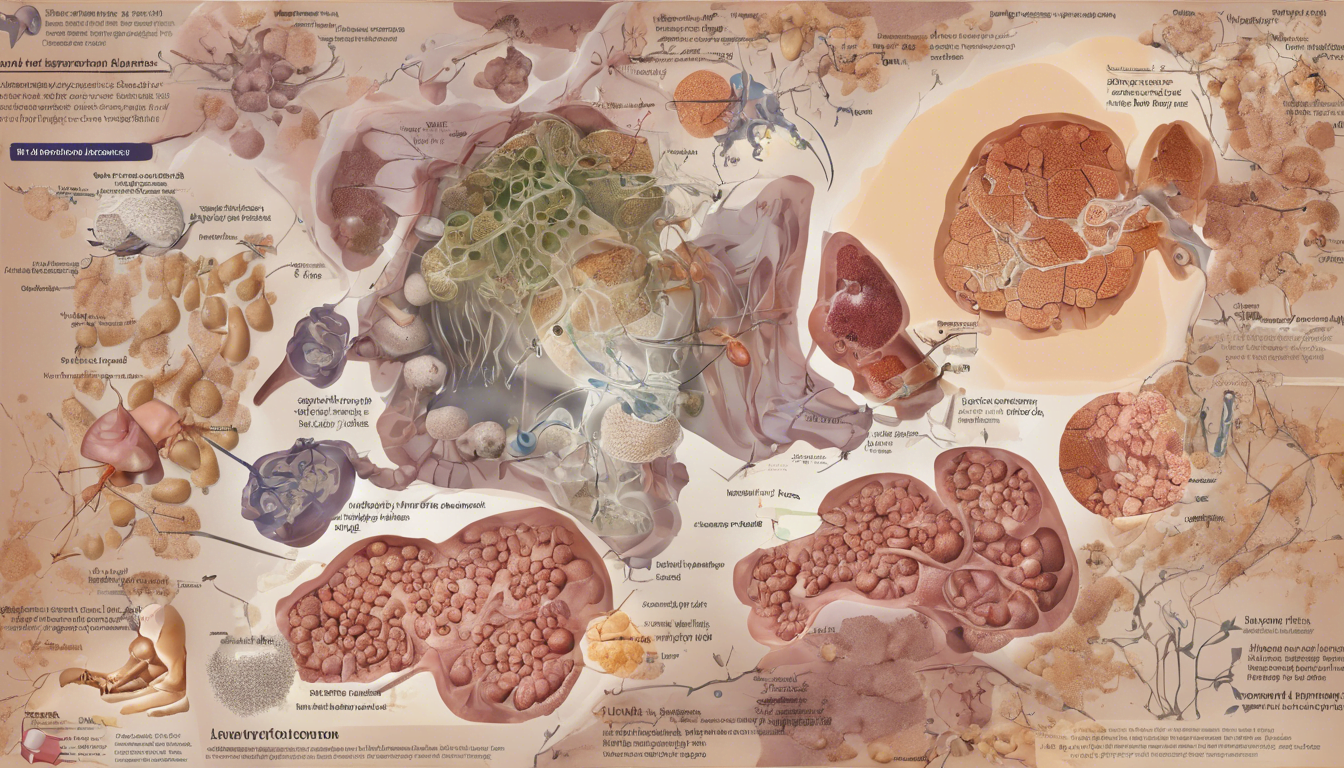
Acute lymphocytic leukemia (ALL), also known as acute lymphoblastic leukemia, is a form of cancer that primarily affects the white blood cells known as lymphocytes. This disease is characterized by the rapid growth of immature lymphocytes, predominantly affecting the bone marrow where these blood cells are produced. In ALL, the bone marrow produces large numbers of abnormal lymphocytes, which are not fully developed and are unable to function properly.
The progression of ALL is swift, and without treatment, it could be fatal within a few months. The term “acute” in acute lymphocytic leukemia signifies the rapid progression of the disease, while “lymphocytic” indicates that the leukemia originates from lymphocytes.
One key aspect of ALL is that it can start from either early B cells or T cells at different stages of their development. These cells are crucial components of the immune system, with B cells producing antibodies and T cells destroying infected or cancerous cells. In ALL, these cells do not mature properly and accumulate, leading to a decrease in the production of healthy blood cells.
The disease can quickly spread beyond the bone marrow to other parts of the body such as the lymph nodes, liver, spleen, central nervous system (including the brain and spinal cord), and, in males, the testicles. This widespread involvement can lead to a variety of symptoms including anemia, infections, and issues related to increased intracranial pressure due to central nervous system involvement.
In the United States, ALL accounts for approximately 2 percent of lymphoid neoplasms and occurs slightly more frequently in males than females. It is also three times more common in Caucasians compared to African Americans. These statistics highlight the demographic variations in the incidence of ALL, which could be crucial for understanding risk factors and tailoring public health interventions.
Understanding acute lymphocytic leukemia involves recognizing its rapid development, the types of cells it affects, and its potential to severely disrupt normal bodily functions. This knowledge is essential for diagnosing the disease early and initiating appropriate treatment strategies to manage and potentially cure it.
Causes and Risk Factors
Understanding the causes and risk factors of acute lymphocytic leukemia (ALL) is crucial for both patients and healthcare providers. The development of ALL can be influenced by a combination of genetic and environmental factors.
Genetic Factors
Several genetic syndromes have been identified that increase the risk of developing ALL. Conditions such as Down syndrome, Klinefelter syndrome, Fanconi anemia, Bloom syndrome, Ataxia-telangiectasia, Neurofibromatosis, and Li-Fraumeni syndrome are known to predispose individuals to this type of leukemia. While not all cases of ALL are inherited, certain inherited DNA mutations can significantly raise the risk. Most DNA mutations related to ALL, however, are acquired during a person’s lifetime and are not inherited from parents.
Environmental Factors
Exposure to high levels of ionizing radiation is a well-documented risk factor for developing leukemia. This includes radiation from sources such as UV rays, X-rays, and nuclear power. Additionally, survivors of atomic bombings have shown a significantly increased risk of developing acute leukemia.
Chemical exposure also plays a role in the onset of ALL. Prolonged exposure to benzene, which is found in cigarette smoke, certain cleaning products, and industrial solvents, has been linked to an increased risk of ALL. Furthermore, exposure to certain chemotherapy drugs used in cancer treatment has been associated with a higher risk of developing leukemia later on.
Environmental factors during early childhood and pregnancy also contribute to the risk. For instance, maternal exposure to pesticides and other chemicals during pregnancy can increase the likelihood of a child developing ALL. Similarly, exposure to low doses of ionizing radiation in early childhood has been convincingly associated with childhood ALL.
In addition to these factors, viral infections such as human T-cell lymphoma/leukemia virus-1 (HTLV-1) and Epstein-Barr virus (EBV) have been linked to increased risks of specific types of ALL, particularly in certain geographic regions.
By understanding these genetic and environmental risk factors, individuals can better assess their own risk and healthcare providers can develop more targeted prevention and treatment strategies for acute lymphocytic leukemia.
Symptoms and Diagnosis
Common Symptoms
Acute lymphocytic leukemia (ALL) manifests through various symptoms, largely due to the shortage of normal blood cells, a result of leukemia cells overcrowding the bone marrow. We might feel tired, weak, or dizzy, and experience shortness of breath and pale skin. Frequent or severe infections that don’t go away, along with unusual bruising or bleeding, such as frequent nosebleeds or heavy menstrual periods, are common. Additionally, symptoms like weight loss, fever, night sweats, and loss of appetite are often reported.
Swelling in the abdomen due to enlarged liver and spleen can cause a feeling of fullness after eating only a small amount. Enlarged lymph nodes, which may appear as lumps under the skin, particularly in the neck, groin, or underarm areas, are also indicative of ALL. Less commonly, ALL can affect the brain and spinal cord, leading to headaches, weakness, vomiting, or blurred vision.
Diagnostic Tests
Diagnosing ALL involves a series of tests. Initially, blood tests might reveal an abnormal count of white and red blood cells and platelets, often showing the presence of blast cells. A bone marrow test, where a sample is extracted from the hipbone or breastbone, is crucial for confirming the presence of leukemia cells.
Imaging tests such as X-rays, CT scans, or ultrasounds determine if the cancer has spread to other parts of the body like the brain and spinal cord. A spinal fluid test, or lumbar puncture, checks if cancer cells have infiltrated the spinal fluid.
Further diagnostic procedures include detailed examinations during a physical check-up, where doctors look for enlarged organs, lymph nodes, and signs of infection. Blood samples are taken for a complete blood count (CBC) to measure the levels of various blood cells and to observe the appearance and characteristics of these cells under a microscope.
For a definitive diagnosis, bone marrow aspiration and biopsy are performed. This procedure not only confirms the presence of leukemia cells but also helps in assessing the response to treatment. Additional tests like flow cytometry and immunohistochemistry help classify leukemia cells based on their surface proteins, aiding in pinpointing the specific type of leukemia.
Treatment Options
Chemotherapy
We often rely on chemotherapy as the primary treatment for acute lymphocytic leukemia (ALL). This method uses various drugs to target and kill cancer cells throughout the body. During the induction phase, the treatment is intensive and may last about a month, followed by consolidation and maintenance phases which are less intensive but longer. Common drugs include Vincristine, Daunorubicin, and L-asparaginase among others. Despite its effectiveness, chemotherapy can cause significant side effects such as hair loss, mouth sores, and a decrease in blood cell counts, which increases the risk of infections.
Stem Cell Transplant
Stem cell transplant is a vital option, particularly for high-risk patients or those who haven’t responded to initial treatments. We use high doses of chemotherapy, sometimes in combination with radiation, to destroy the remaining cancer cells before transplanting healthy blood-forming stem cells into the patient’s body. Allogeneic transplants, where the stem cells are sourced from a donor, are commonly preferred because of their potential to initiate a graft-versus-leukemia effect, which can attack residual cancer cells.
Targeted and Immunotherapy
Advancements in targeted therapy and immunotherapy have provided us with more precise treatment options. Drugs like tyrosine kinase inhibitors specifically target cancer cell growth signals, while monoclonal antibodies like Blinatumomab and Inotuzumab ozogamicin direct the body’s immune response against leukemia cells. CAR T-cell therapy, another innovative approach, involves modifying patient’s T-cells to better identify and destroy cancer cells.
Radiation Therapy
Radiation therapy is not typically a frontline treatment for ALL but is used in specific scenarios such as preventing cancer spread to the brain and spinal fluid or managing tumors causing severe symptoms. It involves directing high-energy radiation beams at targeted areas of the body. While effective in certain cases, the potential long-term side effects, especially in children, such as cognitive and growth impairments, necessitate careful consideration.
Conclusion
Throughout this comprehensive exploration of acute lymphocytic leukemia (ALL), we’ve delved into its complexities, from the initial signs and symptoms to the cutting-edge treatments that offer hope to those affected. Our journey through understanding ALL underscores the importance of early diagnosis, the role of genetic and environmental factors in its development, and the significant advances in treatment options that have transformed patient outcomes. Armed with this knowledge, patients and their families are better positioned to navigate the challenging terrain of ALL, making informed decisions about their healthcare and embracing the progress science offers.
As we conclude, it’s apparent that while the battle against ALL is daunting, the strides made in understanding and treating this disease are monumental, nudging us closer to more personalized and effective care. The implications of these advances extend beyond immediate treatments, opening doors to further research and innovation that promise even greater improvements in the prognosis of ALL patients. In the face of such a complex adversary, the collective efforts of medical professionals, researchers, and communities continue to light the path to a future where acute lymphocytic leukemia can be consistently managed or, optimistically, cured.