Navigating the landscape of acoustic neuroma, a benign but potentially life-altering tumor, requires a comprehensive understanding from diagnosis to treatment. Acoustic neuroma, also known as vestibular schwannoma, affects a critical nerve in the brain, interfacing between the inner ear and the brain, which can lead to significant health implications.
Given its stealthy onset and the array of symptoms it triggers, awareness and early detection are crucial. Our journey through understanding what acoustic neuroma is, recognizing its symptoms, and exploring available treatments is not only aimed at those directly impacted but also at fostering a broader awareness. The fact that even celebrities with acoustic neuroma have brought attention to this condition underscores its relevance and the importance of credible information.
In this article, we delve into the essential aspects of acoustic neuroma, starting with a detailed discussion on what acoustic neuroma is, laying the groundwork for a deeper comprehension. We then guide you through identifying the symptoms of acoustic neuroma, highlighting how they manifest and the potential impact on quality of life.
The diagnostic process, including the role of acoustic neuroma MRI, will be explored to demystify the steps leading to a conclusive diagnosis. Subsequently, our discussion will cover the spectrum of acoustic neuroma treatment options, from monitoring to surgery, providing insights into decision-making and expected outcomes. Finally, we will reflect on the journey of managing acoustic neuroma, underscoring the significance of informed choices in enhancing life expectancy and quality of life for those affected.
What is Acoustic Neuroma?
Definition of Acoustic Neuroma
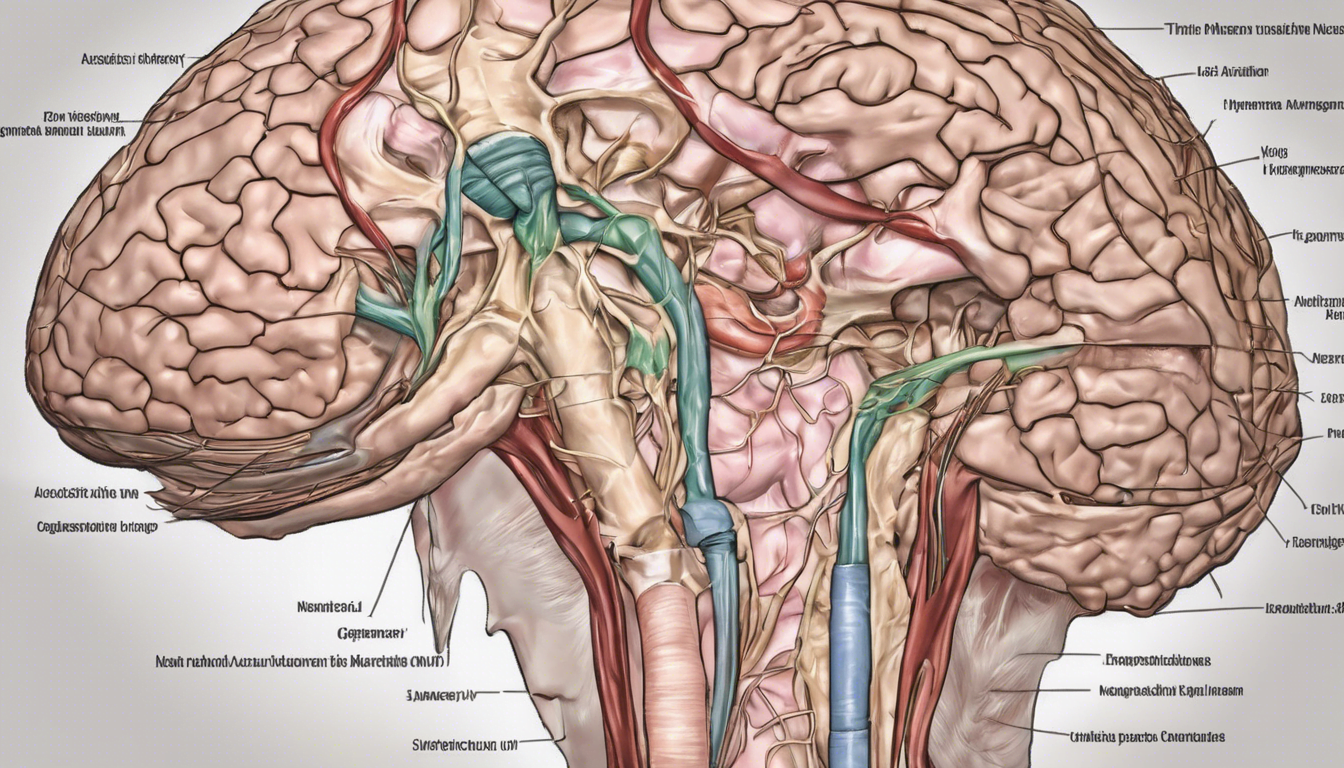
An acoustic neuroma, also known as vestibular schwannoma, is a benign, usually slow-growing tumor that develops from the Schwann cells covering the vestibular nerve, which is part of the cranial nerve that connects the inner ear with the brain. These tumors typically arise where the central nervous system transitions into the peripheral nervous system at the porus acusticus and are most commonly found in the cerebellopontine angle, adjacent to the cochlear or vestibular nerves.
Causes & Risk Factors
The primary cause of acoustic neuromas is often linked to a genetic mutation on chromosome 22, which adversely affects the tumor suppressor protein that controls the growth of Schwann cells. This mutation is particularly associated with neurofibromatosis type 2 (NF2), a rare genetic disorder characterized by the growth of noncancerous tumors on the balance and hearing nerves on both sides of the head. Although environmental factors like radiation exposure have been studied, no definitive link has been established except for radiation, which is known to increase the likelihood of developing these tumors. It is important to note that neurofibromatosis type 2 is the only confirmed risk factor, accounting for about 5% of acoustic neuroma cases.
Types of Acoustic Neuroma
Acoustic neuromas are classified into two types: sporadic and genetic. Sporadic, unilateral acoustic neuromas occur in about 95% of cases and are typically non-hereditary, affecting only one side of the body. These can develop at any age but are most common between the ages of 30 and 60. On the other hand, genetic, bilateral acoustic neuromas are associated with NF2 and involve tumors on both sides of the head. This type is less common but significantly impacts patients due to the multiple tumors that can develop throughout the body, often requiring different treatment approaches.
Symptoms of Acoustic Neuroma
Hearing Loss
Hearing impairment is the most prevalent symptom of acoustic neuroma, affecting up to 90% of patients. This hearing loss typically manifests unilaterally, meaning it occurs in one ear, which gradually worsens over time. In some cases, individuals might experience sudden hearing loss, which can fluctuate—improving and then worsening again. People with this condition often find it challenging to hear in noisy environments or to pinpoint the direction from which sounds are coming.
Tinnitus
Tinnitus, or ringing in the ears, is another common symptom associated with acoustic neuroma, occurring in many patients. This symptom is typically experienced as a high-pitched tone in the affected ear, although it can also present as hissing, buzzing, or roaring sounds. For some, tinnitus may be constant, while for others, it can come and go, varying in intensity.
Balance Issues
Nearly half of all individuals with an acoustic neuroma experience balance problems due to the tumor’s impact on the vestibular nerve, which is integral to maintaining equilibrium. Symptoms can range from mild unsteadiness to severe balance difficulties, potentially leading to falls, particularly as the tumor grows. While true vertigo is not common, some patients may experience a sensation of spinning or tilting due to changes in tumor size or associated bleeding.
Facial Numbness
Facial numbness or tingling, often intermittent, can occur when an acoustic neuroma presses against the trigeminal nerve. This symptom may be localized to areas like the corner of the mouth or cheek. In advanced cases, the tumor’s growth can lead to more severe effects such as facial weakness or paralysis if it compresses adjacent cranial nerves.
Diagnosis of Acoustic Neuroma
Physical Examination
The initial approach in diagnosing an acoustic neuroma often involves a thorough physical examination, particularly focusing on the ears. After discussing symptoms, a healthcare professional performs an ear exam to check for any abnormalities that could indicate the presence of a tumor. This step is crucial as early symptoms of acoustic neuroma can be subtle and are commonly associated with other middle and inner ear issues.
Audiometry
Audiometry is a critical diagnostic tool used to assess hearing function. During this test, an audiologist presents a range of sounds at various tones to one ear at a time. The patient indicates whenever they hear a sound, helping to determine the softest level of sound they can detect. Speech audiometry may also be conducted to evaluate how well patients can understand words. This test is particularly important as acoustic neuromas often lead to asymmetric unilateral hearing loss, which can be an early indicator of the condition.
Imaging Studies
MRI scans are the cornerstone of acoustic neuroma diagnosis. These scans use magnetic fields and radio waves to create detailed images of the brain and are particularly effective when combined with a contrast dye, which helps to highlight the tumor against surrounding tissues. In cases where MRI is not suitable, such as in patients with pacemakers, CT scans are used as an alternative, though they are less sensitive in detecting small tumors. High-resolution T2-weighted imaging offers an alternative method, providing detailed views of the nerve structures within the internal auditory canal and helping to evaluate the extent of tumor involvement.
Treatment Options for Acoustic Neuroma
Observation
Observation, often referred to as the “watch-and-wait” approach, is increasingly utilized, especially when acoustic neuromas are identified early and are not causing significant symptoms. This method involves regular monitoring through imaging studies, such as MRI, to track any changes in the tumor’s size or behavior. Typically, we recommend follow-up visits every six to twelve months, although the frequency can increase if any tumor growth is detected. Observation is particularly considered for patients who are elderly or have other health conditions that increase the risks associated with surgery.
Surgery
Surgical removal of the tumor remains a cornerstone of acoustic neuroma treatment, particularly for tumors that are large or symptomatic. The goal of surgery is to remove as much of the tumor as possible while striving to preserve neurological function, including hearing and facial nerve integrity. There are several surgical approaches:
- Retrosigmoid Approach: This method allows access to the tumor via an incision behind the ear, suitable for various tumor sizes and potentially preserving hearing.
- Translabyrinthine Approach: Used primarily for larger tumors or when hearing preservation is not feasible. This approach provides excellent access to the tumor and early visualization of the facial nerve.
- Middle Fossa Approach: Ideal for smaller tumors located primarily within the internal auditory canal, this approach offers the best chance of preserving hearing.
Each surgical method involves detailed imaging to guide the procedure and monitor vital nerve functions throughout.
Radiation Therapy
For patients where surgery is deemed too risky or in cases where the tumor is not completely resectable, radiation therapy offers a non-invasive alternative to control tumor growth. Techniques such as stereotactic radiosurgery (SRS) and fractionated stereotactic radiotherapy (FSR) are commonly employed. These methods involve delivering focused radiation to the tumor, minimizing exposure to surrounding healthy tissues:
- Stereotactic Radiosurgery: Utilizes precise beams of radiation, commonly through systems like Gamma Knife or CyberKnife, targeting the tumor with minimal impact on adjacent structures.
- Fractionated Stereotactic Radiotherapy: Delivers smaller doses of radiation over several sessions, which can be beneficial for larger tumors or when minimizing long-term side effects is a priority.
Radiation therapy is chosen based on factors such as the tumor’s size, location, and the patient’s overall health and age. The aim is to achieve tumor control while preserving as much neurological function as possible.
Conclusion
Through our exploration of acoustic neuroma, we’ve journeyed from its basic understanding, symptom recognition, to the intricacies of diagnosis and treatment options, highlighting the importance of early detection and informed decision-making. The discussion emphasized that while acoustic neuroma presents significant challenges, the advances in diagnostic techniques and treatment methodologies offer hope and improved outcomes for those affected. Moreover, the emphasis on patient-centered care – considering the individual’s health status, tumor characteristics, and personal preferences in treatment planning – underscores the evolution towards more personalized and effective management strategies.
The insights provided into the potential impacts of acoustic neuroma, coupled with treatment advancements and the critical role of informed choices, not only aim to enhance quality of life but also serve as a call to action for ongoing awareness and patient education. Recognizing the significance of this condition in the broader spectrum of neurological disorders encourages further research and underscores the continual need for innovation in treatment and management practices. Ultimately, the journey through understanding and managing acoustic neuroma is one of resilience, collaboration, and hope, guiding patients towards a path of better health and well-being.
FAQ on Acoustic Neuroma
1. What is acoustic neuroma and what causes it?
Answer: Acoustic neuroma, also known as vestibular schwannoma, is a benign tumor that develops on the vestibular nerve, which connects the inner ear to the brain. The primary cause is often linked to a genetic mutation on chromosome 22, particularly associated with neurofibromatosis type 2 (NF2). While environmental factors like radiation exposure have been studied, NF2 is the only confirmed risk factor, accounting for about 5% of cases.
2. What are the common symptoms of acoustic neuroma?
Answer: Common symptoms include:
- Hearing Loss: Unilateral (one ear) hearing impairment, which may be gradual or sudden.
- Tinnitus: Ringing, buzzing, or hissing sounds in the affected ear.
- Balance Issues: Unsteadiness or balance difficulties, potentially leading to falls.
- Facial Numbness: Tingling or numbness in the face, which may progress to facial weakness or paralysis in advanced cases.