When we discuss conditions that could potentially alter the course of our lives, abdominal aortic aneurysm (AAA) stands prominently among them. This serious medical condition, often silent in its progression, can have dire consequences if not identified and treated promptly. Understanding what causes abdominal aortic aneurysms, recognizing the symptoms, and knowing the available treatment options can significantly impact outcomes for those at risk. Our health and well-being are paramount, and being informed about conditions like AAA is a crucial step in safeguarding them.
In this article, we will dive deep into the anatomy of an abdominal aortic aneurysm, exploring its primary causes and risk elements that contribute to its development. We will delineate the symptoms of abdominal aortic aneurysm, emphasizing the importance of early detection through abdominal aortic aneurysm screening and diagnosis methods such as abdominal aortic aneurysm ultrasound and radiology.
Our discussion will extend to the available treatments, from monitoring strategies for an infrarenal abdominal aortic aneurysm to the surgical interventions required for a ruptured abdominal aortic aneurysm. By shedding light on these critical aspects, we aim to empower our readers with knowledge that can aid in the prevention, early detection, and management of AAA.
Defining Abdominal Aortic Aneurysm
What is AAA?
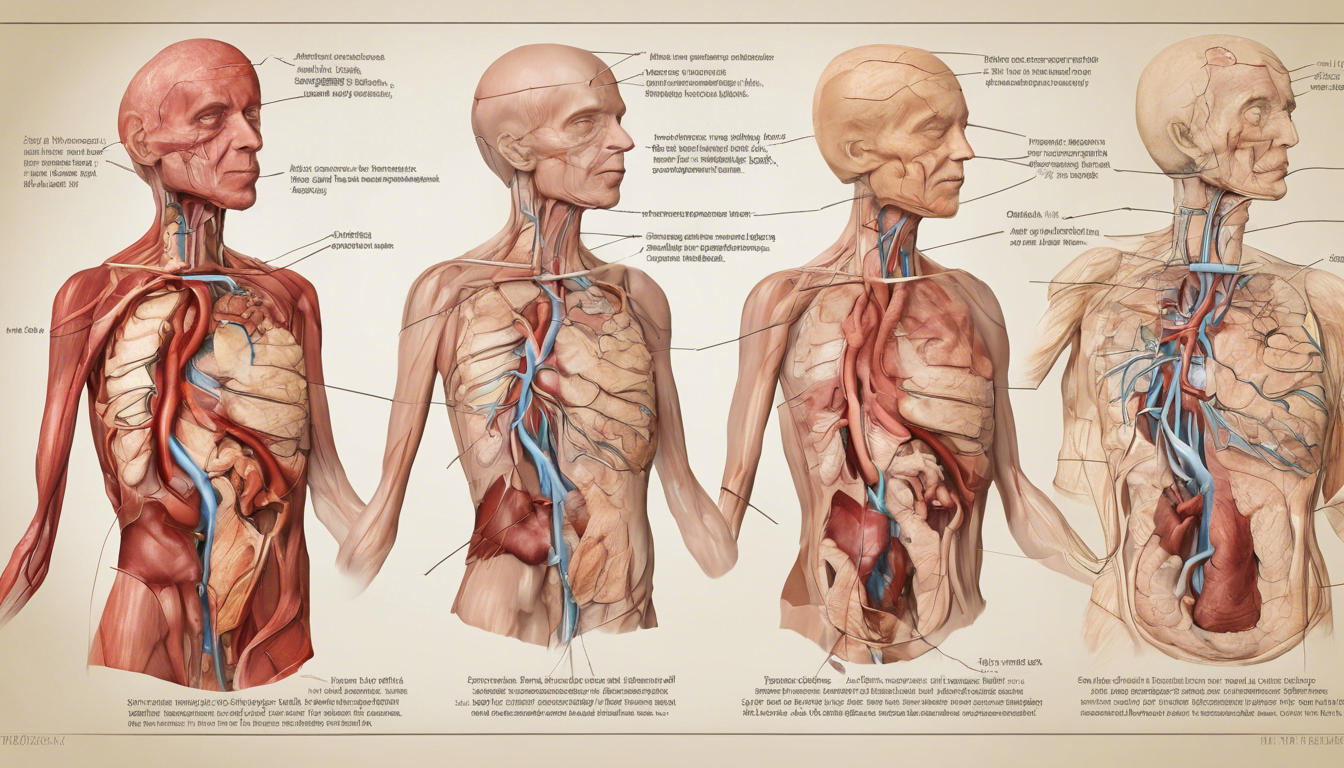
An abdominal aortic aneurysm (AAA) is characterized as a permanent focal dilation of the abdominal aorta, where the diameter is at least 50% greater than the normal adjacent sections. This condition predominantly affects the segment of the aorta below the renal arteries, known as the infrarenal aorta.
Anatomy of the Aorta
The aorta, the largest blood vessel in the body, begins at the heart’s left ventricle and extends upwards to form an arch before descending through the chest into the abdomen. As it travels downward, it narrows and branches out to supply vital organs and other body parts with oxygen-rich blood. The abdominal aorta specifically enters the abdomen under the median arcuate ligament, lying anterior and slightly to the left of the lumbar vertebrae, eventually dividing into the iliac arteries just above the pelvis.
Frequency and Demographic Details
Abdominal aortic aneurysms are relatively common, especially in individuals over the age of 65, with a prevalence of about 7.5%. Autopsy studies show that the frequency of these aneurysms varies between 0.5% to 3%, peaking in the seventh and eighth decades of life. The condition is notably more prevalent in white males and those with a history of smoking, which significantly increases the risk due to the weakening of the arterial walls.
Primary Causes and Risk Elements
Smoking and genetics are pivotal in the development of an abdominal aortic aneurysm (AAA). Research indicates that smoking, particularly current smoking, has a profound impact on the prevalence of AAA, more so in females than in males. The correlation between obesity and AAA is also significant, likely due to adipokines and obesity-induced aortic inflammation that weakens the vessel, leading to aneurysmal formation.
Genetic predispositions combined with environmental factors play a crucial role in the development and progression of AAA. Familial history is a significant risk factor, with a notable increase in risk for individuals who have a first-degree relative with an AAA.
Medical conditions such as chronic obstructive pulmonary disease (COPD), atherosclerosis, and hypertension are commonly associated with AAA. These conditions contribute to the weakening of the aortic wall, exacerbating the risk of aneurysm. Additionally, factors like high blood pressure and certain bacterial infections can further compromise aortic integrity, increasing the likelihood of an AAA.
Gender and age are non-modifiable risk factors that influence the prevalence and characteristics of AAA. Males, especially those over the age of 65, are more prone to developing AAA. Interestingly, while AAA is less common in females, the aneurysms tend to exhibit higher peak wall stress and faster growth rates in the aortic wall once an AAA develops. This suggests a need for gender-specific guidelines in screening and management of AAA.
Through understanding these primary causes and risk elements, we can better approach the prevention and early detection of AAA, potentially reducing the adverse outcomes associated with this condition.
Symptoms to Watch For
Common Locations of Pain
Abdominal aortic aneurysms (AAA) often manifest as pain, which is the most common symptom. This pain may be located in the abdomen, chest, lower back, or groin area. It can vary from being severe to dull. Specifically, individuals might experience steady, deep pain in the lower back or belly, and pain may also spread to the leg, groin, or pelvic area.
Symptoms of a Large or Growing Aneurysm
As an AAA enlarges, it may cause deep, constant pain in the belly area or side of the belly, and back pain. A distinctive pulse near the bellybutton can often be felt, which may resemble a heartbeat. This pulsing sensation in the abdomen is a critical sign of a growing aneurysm.
Emergency Signs of AAA Rupture
The rupture of an AAA presents with sudden, intense, and persistent symptoms. These include severe belly or back pain, which may feel like ripping or tearing, accompanied by low blood pressure and a fast pulse. Such a scenario demands immediate medical attention as it is life-threatening. If you experience these symptoms, especially if they are sudden and severe, it is crucial to seek emergency medical help right away.
Subtle Signs and Routine Checkups
Interestingly, about 75% of AAAs do not cause symptoms and are often discovered incidentally during examinations for other unrelated issues. However, subtle signs might include general belly discomfort, which may come and go or be constant. Symptoms might also include a pulsating feeling in the belly, often without other noticeable changes. Due to the asymptomatic nature of many aneurysms, routine screening, especially for men aged 65 to 75 who have smoked, is recommended. This screening usually involves an ultrasound of the abdomen to check for aneurysms.
Diagnosing AAA
Physical Examinations and History
In the process of diagnosing an abdominal aortic aneurysm (AAA), a thorough physical examination and review of the patient’s medical and family history are crucial. Most clinically significant AAAs are palpable upon routine examination, depending on the examiner’s experience, the aneurysm’s size, and the patient’s physique. The presence of a pulsatile abdominal mass is a strong indicator of AAA, although it is detected in fewer than half of the cases. Additionally, differences in upper-extremity blood pressures may suggest subclavian artery stenosis, which is important to note during perioperative monitoring.
Utility of Imaging Tests (CT, MRI, X-rays)
Imaging plays a pivotal role in the AAA diagnostic process. Abdominal ultrasound is commonly used due to its high sensitivity and specificity. However, for more detailed information, especially in symptomatic patients, computed tomography (CT) or magnetic resonance imaging (MRI) may be employed. These methods provide superior image quality, allowing for precise measurements of the aneurysm’s size and shape, and can identify rapid expansion or rupture. While CT offers detailed images and is less operator-dependent, its use is generally limited as a screening tool due to radiation exposure.
Benefits of Screening Programs
Screening programs for AAA have shown significant benefits, particularly in reducing mortality and emergency surgeries. Large-scale studies, such as those conducted in Oslo, have demonstrated the effectiveness of screening 65-year-old men using ultrasound, significantly lowering the AAA-related mortality and rupture rates. The European Society for Vascular Surgery recommends one-time ultrasonographic screening for all men at the age of 65, with follow-up scans for those with detected aortic dilatation.
Medical Consultation and Specialist Care
Upon detection of an AAA, it is crucial for patients to receive appropriate medical consultation and specialist care. General practitioners (GPs) typically manage the surveillance of detected AAAs until a certain threshold, after which referral to a specialized center like Oslo University Hospital is necessary for further evaluation and potential treatment. This structured referral and treatment pathway ensures that patients receive timely and effective intervention, minimizing the risks associated with AAA progression.
Conclusion
Throughout this article, we’ve traversed the intricate landscape of abdominal aortic aneurysms, from their underlying causes and risk factors to the warning signs and diagnostic pathways that can lead to timely intervention. By highlighting the fundamental anatomy, demographic trends, and the imperative for early detection through screening, we’ve aimed to underscore the importance of awareness and proactive healthcare. The discussion on treatment options, from surveillance to surgical intervention, provides a beacon of hope for individuals at risk, illuminating the path to potentially life-saving solutions.
The gravity of abdominal aortic aneurysms cannot be overstated, given their capacity to alter the course of lives silently and swiftly. Recognizing the symptoms, understanding the risk factors, and adhering to recommended screening guidelines can significantly mitigate the threats posed by this condition.
As we conclude, let us carry forward the knowledge that being informed is the first step in prevention and that early detection coupled with modern medical interventions can vastly improve outcomes for those affected by AAA. The collective efforts in research, as well as patient and practitioner education, are pivotal in continuing to combat the prevalence and impact of abdominal aortic aneurysms.
FAQ about abdominal aortic aneurysms (AAA):
What is an abdominal aortic aneurysm (AAA)?
- An AAA is a permanent dilation of the abdominal aorta where the vessel diameter is at least 50% greater than normal. It primarily affects the segment below the renal arteries.
2. What causes AAA?
- Causes include smoking, genetic predispositions, medical conditions like atherosclerosis, hypertension, and chronic obstructive pulmonary disease (COPD). Obesity and certain bacterial infections also increase risk.
3. Who is at risk for AAA?
- Men over 65, particularly those who have smoked, are at higher risk. AAAs are more common in white males and individuals with a family history of the condition.
4. What are the symptoms of AAA?
- Symptoms may include deep, constant pain in the abdomen, chest, lower back, or groin, and a pulsating sensation near the bellybutton. However, many AAAs are asymptomatic and discovered incidentally.