In the landscape of pulmonary diseases, centrilobular emphysema stands as a significant contributor to respiratory morbidity, deserving our focussed attention. As a distinct form of chronic obstructive pulmonary disease (COPD), it particularly affects the central parts of the lung lobules.
Its importance cannot be understated, as understanding this condition is pivotal in managing the health outcomes of a considerable segment of the population. With advancements in diagnostic techniques and treatment modalities, our approach to centrilobular emphysema—or central lobular emphysema and even centriacinar emphysema, as it’s variably known—has evolved, underscoring the need for updated insights on its management.
In this article, we aim to dissect the nuances of diagnosing centrilobular emphysema, closely followed by a thorough discussion on the symptoms that herald its presence, and the contemporary strategies employed in its treatment.
Our coverage extends from the clinical presentation and the application of the centrilobular emphysema icd 10 classification in diagnosis, through to the latest in treatment and management, providing a holistic view on the condition. We are committed to offering a detailed roadmap that elucidates the challenges and solutions associated with centrilobular emphysematous disease, aiming to enhance patient care and outcomes.
Overview of Centrilobular Emphysema
Historical Background
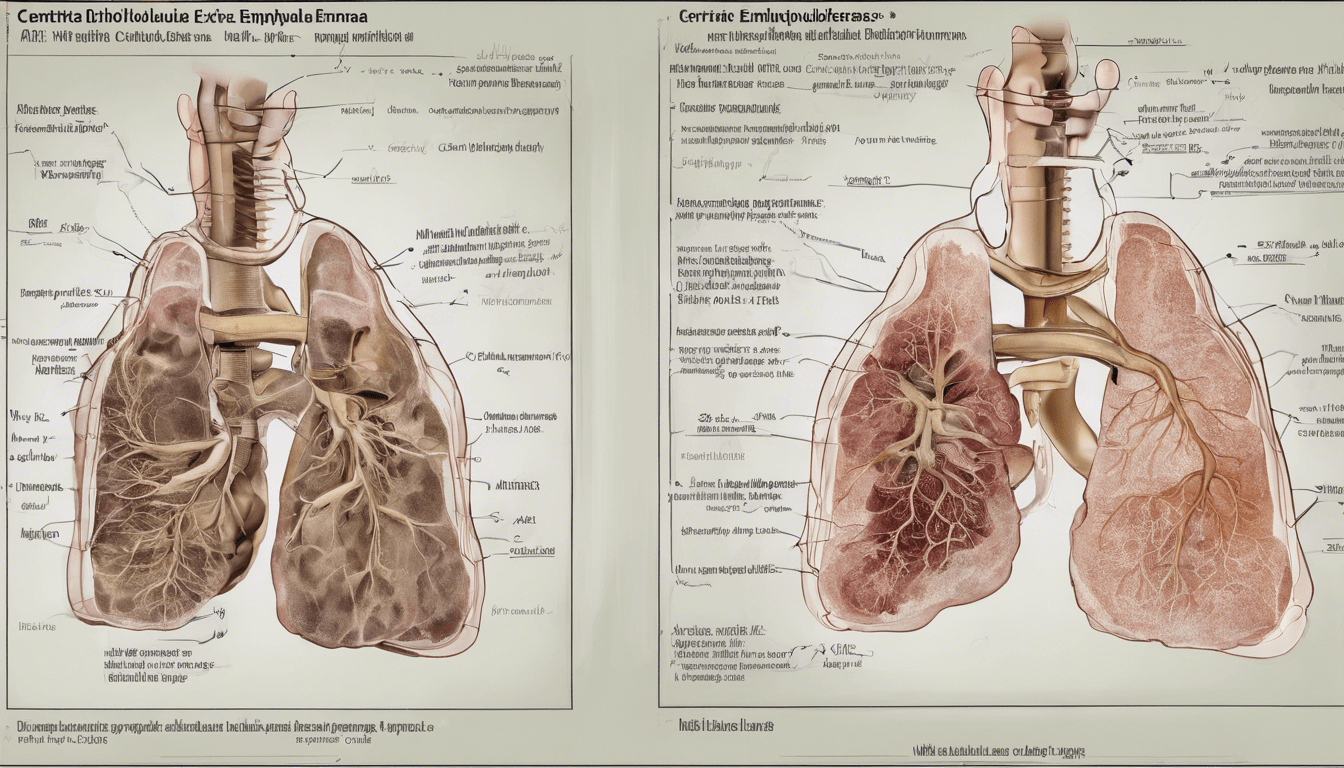
Centrilobular emphysema, also known as centriacinar emphysema, predominantly affects individuals over the age of 50 who have a history of smoking. This condition is characterized by damage that begins in the central parts of the lung’s secondary pulmonary lobules, unlike panlobular emphysema, which affects tissues throughout the lungs simultaneously.
Pathogenesis
The pathogenesis of centrilobular emphysema involves the inhalation of harmful chemicals found in cigarette smoke, which lead to inflammation and the destruction of the lungs’ small air sacs. This damage primarily occurs in the upper lobes of the lungs and obstructs the flow of air, making breathing difficult. Additionally, exposure to other toxic inhalants, such as coal dust or vehicle exhaust, can exacerbate this condition, particularly in certain occupational settings.
Classification
Centrilobular emphysema is classified based on the appearance of low attenuation areas (LAA) on high-resolution computed tomography (HRCT). These areas can vary in shape and border sharpness, leading to their classification into three types: Type A (round or oval with well-defined borders), Type B (polygonal or irregular with ill-defined borders, less than 5 mm in diameter), and Type C (irregular with ill-defined borders, 5 mm or over in diameter).
Most patients exhibit one dominant type of LAA, which correlates with varying degrees of airflow limitation and diffusion capacity in pulmonary function tests.
Diagnostic Approach
Clinical Evaluation
To accurately diagnose centrilobular emphysema, we often begin by assessing the progression of the disease. This involves a thorough clinical evaluation to understand the symptoms and history of exposure to risk factors such as smoking or occupational hazards.
Functional Assessment
Several tests are crucial for the functional assessment of lung capabilities. We utilize spirometry testing to measure the volume of air a person can expel from the lungs and the speed of the exhalation.
Plethysmography is another key test, used to assess total lung capacity by having the patient breathe in a sealed chamber. Additionally, a pulse oximetry test may be conducted to measure the oxygen saturation in the blood, providing insights into the lungs’ efficiency at gas exchange.
Imaging Techniques
High-resolution computed tomography (HRCT) is indispensable in our diagnostic toolkit. It helps in identifying the morphological characteristics of centrilobular emphysema, such as low attenuation areas (LAA) which can vary in shape and border definition. These LAAs are classified into three types based on their appearance on HRCT, providing us with detailed insights into the extent and type of lung damage.
Furthermore, HRCT assists in the phenotyping of COPD, distinguishing between primarily parenchymal versus airway diseases, and aids in the assessment of disease severity. This imaging technique, coupled with its ability to visualize the pulmonary arteries and bronchioles, enhances our understanding of the disease’s progression and helps tailor our approach to each patient’s condition.
Treatment and Management
Lifestyle Modifications
Our approach to managing centrilobular emphysema includes several lifestyle changes to prevent the disease from worsening. We recommend quitting smoking as it significantly improves oxygen intake and breathing. To protect your lungs from further damage, getting vaccinated against influenza and pneumococcal diseases is crucial.
Additionally, regular gentle exercises like gardening or slow walks can enhance muscle strength and improve endurance, helping to reduce shortness of breath. For individuals exposed to lung irritants at work, we advise wearing protective masks and discussing environmental adjustments with employers.
Pharmacologic Treatment
Pharmacological management plays a critical role in alleviating symptoms and slowing disease progression. We prescribe a combination of bronchodilators and anti-inflammatory medications to improve airflow and reduce lung inflammation. Medications such as beta-agonists and anticholinergics are used to relax bronchial muscles and improve air passage.
Corticosteroids are another vital component, administered through inhalers to help prevent acute flares and ease breathing. For ongoing management, long-acting bronchodilators combined with inhaled corticosteroids are recommended to maintain open airways and manage symptoms effectively.
Surgical Options
For severe cases of centrilobular emphysema, surgical interventions may be considered. Lung volume reduction surgery (LVRS) is an option for patients with advanced disease, where damaged lung tissue is removed to allow the remaining lung to function more efficiently.
This procedure is typically recommended for individuals who have not responded adequately to medical treatments and exhibit specific disease characteristics as determined through detailed medical evaluations. In cases where lung damage is extensive and other treatments have failed, lung transplantation may be considered to improve breathing and quality of life.
Conclusion
Throughout this article, we have explored the intricate dimensions of diagnosing, understanding the symptoms of, and treating centrilobular emphysema—a condition that poses significant challenges but also presents opportunities for management and intervention.
From the initial steps of recognizing the clinical and diagnostic features, including the use of HRCT for a detailed assessment of lung damage, to the judicious application of both lifestyle modifications and pharmacologic treatments aimed at managing and potentially mitigating the condition’s impact, the pathway to managing centrilobular emphysema requires a comprehensive and informed approach.
The evolution of treatment and diagnostic modalities signifies a beacon of hope for patients grappling with this form of COPD, highlighting the importance of early detection and personalized treatment plans.
Emphasizing the imperative of cessation of smoking, along with strategic pharmacological and, if necessary, surgical interventions, offers a framework within which patients can find relief and a better quality of life.
The journey through understanding and managing centrilobular emphysema underscores the critical importance of patient engagement, clinical innovation, and continued research in advancing our capabilities to combat this debilitating disease effectively.
FAQ on Centrilobular Emphysema
1. What is centrilobular emphysema?
Answer: Centrilobular emphysema is a type of COPD that affects the central parts of the lung lobules, mainly due to smoking, causing airflow obstruction and breathing difficulties.
2. How is centrilobular emphysema diagnosed?
Answer: It is diagnosed through clinical evaluation, spirometry, plethysmography, pulse oximetry, and high-resolution computed tomography (HRCT) to identify lung damage.
3. What lifestyle changes can help manage centrilobular emphysema?
Answer: Quitting smoking, getting vaccinated, exercising regularly, and protecting lungs from irritants are crucial lifestyle changes for managing the condition.
4. What medications are used to treat centrilobular emphysema?
Answer: Treatments include bronchodilators to relax airway muscles, corticosteroids to reduce inflammation, and combination therapies for long-term management.
5. When is surgery considered for centrilobular emphysema?
Answer: Surgery, such as lung volume reduction or lung transplantation, is considered for severe cases where other treatments are ineffective.




1 Comment